Strategies for dealing with health problems and improving healthcare services have been published for England, Wales, Scotland and Northern Ireland. They contain many common elements, such as commitments to reduce avoidable illhealth, with particular emphasis on cancer, heart disease and mental health, improving clinical performance through a more integrated and inclusive network of local health provision, and tackling the various health inequalities which exist across the United Kingdom.
2. The National Health Service
3. Treatment of patients from foreign countries
Overall quality of life has improved considerably in Britain as a result of a number of major social and economic trends, including an increase in real incomes, improvements in nutrition and housing, higher levels of education, improved health services, and developments in medicines and their wider availability to the population.
Life Expectancy
Life expectancy is a useful indicator of mortality. It is a widely used measure of the state of the nation’s health. Since the middle of the 19th century the expectation of life at birth for both females and males has almost doubled. Neither women nor men born in England and Wales in 1841 had an average life expectancy from birth much beyond 40, mainly because of high infant and child mortality. By 1998 the life expectancy at birth for females in Great Britain had reached almost 80, and for males nearly 75 years. However, life expectancy takes no account of quality of life.
Cancer
About a third of the population develop cancer at some time in their lives. Over the 20th century cancer has become more prominent as a cause of death when compared with other major causes. While death rates from some other major types of illness have fallen considerably, those from cancer have not done so to the same extent. Lung cancer among men has fallen dramatically, mainly because fewer men now smoke.
Abortion
Unlike in Hungary where women can request an abortion up until the completion of the first trimester (12 weeks), in Britain they can have an abortion even in the the 24th week of pregnancy. (In the US women have the right to terminate the life of their baby any time throughout pregnancy without having to justify their decision. The price of an abortion, however, goes up manyfold once the firts trimester is up.) In two cases this time limit does not apply: when the baby is certain to have some serious developmental problem, or when the pregnancy poses a grave risk for the mother's health.
Alcohol
Excessive alcohol consumption leads to ill health, and an increased likelihood of problems such as high blood pressure, cancer and disorder of the liver. In 2004–05, around two-fifths of men aged 16 and over and a fifth of women aged 16 and over in the UK had exceeded the recommended amount of alcohol on their heaviest drinking day in the week prior to being interviewed.
Smoking
More cancer deaths in the UK can be attributed to smoking tobacco than to any other single risk factor. The Health Education Authority estimated that smoking was the direct cause of 100,000 deaths in the past year. The prevalence of smoking also varies by social class. For both men and women, the proportion of smokers is higher among those in the manual socio-economic groups than among those in the professional groups.
Drugs
The misuse of drugs is both a serious social and health problem. Results from the 2004/05 British Crime Survey indicate that 16 per cent of men and 9 per cent of women aged 16 to 59 in England and Wales had taken an illicit drug in the previous year. Young people were more likely than older people to misuse drugs; 33 per cent of men and 21 per cent of women aged 16 to 24 had done so in the previous year. Cannabis remained the most commonly used drug among young people, used by 30 per cent of men and 18 per cent of women in the previous year.
Diet
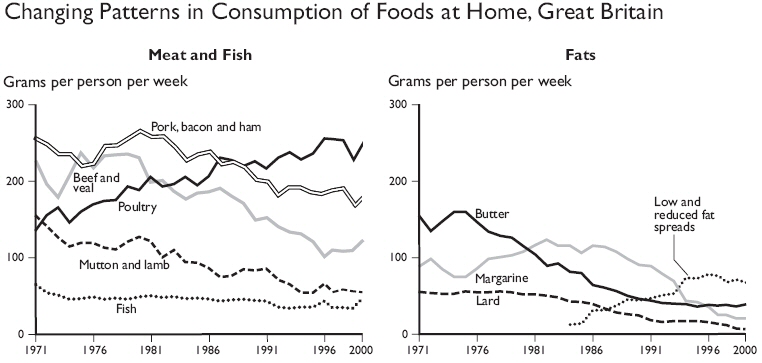
Since the early 1970s there have been marked changes in the British diet. One feature has been the long-term rise in consumption of poultry, while that of red meat (such as beef and veal) has fallen (see Figure). Consumption of fresh fruit has increased since 1970, while consumption of fresh green vegetables was lower in 2000 than in 1970. In addition, the use of convenience food - both frozen and ready meals - has increased. Despite these changes, the British diet is still noticeably different from that in other countries such as those in the Mediterranean, being relatively low in fruit, vegetables and fish. In 1997, three-quarters of children aged 4 to 18 had not eaten any citrus fruits (excluding fruit juice) during the seven-day dietary record, and three-fifths had not eaten any leafy green vegetables. Health considerations appear to have been influencing some aspects of diet in recent years, such as the fall in sales of red meat and the rise in consumption of low-fat spread. However, the proportion of adults who are obese or overweight has increased - in 1999, 19% of women and 21% of men aged 16 and over in England were classified as obese, compared with 8% and 6% respectively in 1980 in Great Britain. The likelihood of being obese increases up to the age of 65 and then declines at older ages.
The structure of the NHS in England and Wales was established by the National Health Service Act 1946 and the new arrangements were launched in 1948. This was under the Welsh health and housing minister Aneurin Bevan. The body responsible for public health in the UK is the National Health Service (NHS).
The NHS is founded on the principle of providing a universal service to all its resident population (even people temporarily resident or visiting the country), based upon need rather than ability to pay. The services are intended to
|
Doctors
Private Treatment |
provide treatment and care where necessary while making the best use of the resources available. The organisation provides the majority of healthcare in the UK, from general practitioners (GPs) to Accident and Emergency Departments, long-term healthcare and dentistry. The NHS is financed mainly through general taxation, along with an element of National Insurance contributions paid by employed people, their employers and selfemployed people. All taxpayers, employers and employees contribute to the cost so that members of the community who do not require healthcare help to pay for those who do. Most forms of treatment are provided free, but some involve a charge, such as prescription drugs (which are subsidised), optician services and dentistry.
The Department of Health (DH) is responsible for national strategic planning in England and for developing and implementing policies for the provision of health services. (The National Assembly for Wales, the Scottish Executive Health Department and the Department of Health, Social Services and Public Safety in Northern Ireland have similar responsibilities for health provision in their respective countries.)
|
Health Inequalities In July 2000, the Government gave a commitment in the NHS Plan that, for the first time ever in England, local targets for reducing health inequalities would be reinforced by the creation of national health inequalities targets: starting with children under one year, by 2010 to reduce by at least 10% the gap in mortality between manual groups and the population as a whole; and by 2010 to reduce by at least 10% the gap between the areas with the lowest life expectancy at birth and the population as a whole. |
Some of the key targets in NHS (improvement) plan:
§ patients to be able to see a GP within 48 hours;
§ waiting time in accident and emergency departments in hospitals to fall to 1 hour 15 minutes on average.
§ the replacement of waiting lists for appointments and admission by booking systems;
§ a reduction in the maximum waiting time for a routine outpatient appointment from six to three months; and
§ a reduction in the maximum waiting time for inpatient treatment from 18 to six months.
Organisation of the NHS
Hospitals are administered by NHS Trusts. GPs remain the 'gatekeepers' to most health care which means that one can only visit specialists if he/she is referred by them. However, new services using telephone and internet channels ("NHS Direct") have recently been developed in response to demands for more flexible sources of advice. Like many other countries, Britain reflected the "end of the hospital" thinking of the 1980s and 1990s and reduced hospital bed capacity to reflect the big increase in day care surgery. The other big capacity constraint is doctors and nurses - Britain does not train enough of them. It is obviously for lack of appropriate financial motivation that there aren't enough medical students to begin with.
Strengths of the National Health System
-
Relatively egalitarian, universal access.
-
Low administrative costs. Around 5 per cent of total health spending goes on administration compared to roughly 20 per cent in the US or Slovakia where instead of the NHS system they have private health insurances.
-
Performance comparisons between hospitals available for anyone to read.
Weaknesses
-
Under-investment in buildings, equipment and doctors has left the system struggling to attain the levels demanded by an increasingly affluent population.
-
Lack of choice for patients and lack of competition means there is not enough motivation for NHS providers to respond to 'consumer demand' or improve the experience of patients.
-
Perversely, the longer the waiting lists the higher the government fundings. (The more the system 'fails' the more it will be rewarded by the state. No incentive to improve!)
Treatment of patients from foreign countries
Hospitals and medical treatment
§ Dial 999 for an ambulance in case of an emergency
§ Emergency medical treatment is free
§ Additional medical care can be very expensive
§ It is advised for everyone to have a medical insurance (one that includes special transport back to your country if needed)
Pharmacists
You can buy a wide range of proprietary medicines without prescription from chemists in Britain. Many medicines, however, are only available with a doctor's prescription, which you must take to a dispensing chemist or pharmacist. If you are likely to need drugs, either bring your own or get your doctor to write out the generic name of the drug. If you are entitled to an Pharmacy NHS prescription, you will be charged a standard rate; without this entitlement you will be charged the full cost of the drug. Remember to ask for a receipt for any insurance claim.
Some pharmacies are open until midnight; for emergencies contact the local hospital. Doctors' surgeries are normally open mornings and early evenings. You can turn up at a hospital casualty department any time. In an emergency, dial 999 for an ambulance.
As an alternative to the NHS, people are entitled to pay for their own health and social care, by joining a private healthcare organisation. In addition, there is the option of private medical insurance, which, depending on the premium paid, will cover people’s healthcare in times of need. In 2000, 11.5% of the population of the United Kingdom were covered by private medical insurance. The major difference between the NHS and the private medical services is not the quality but the time-spam one should wait for the service. NHS patients who do not need an urgent operation have to wait for months or even more than a year, and even those whose case is more serious sometimes have to wait more than a month - this is how the waiting list operates. In the private healthcare system patients can choose the time of their operation; whenever and as soon as they want. Private patients may use so called 'pay beds' usually in a separate room in NHS hospitals (there are of course completely private hospitals and clinics), while NHS patients are placed in rooms with as many as ten or more beds.
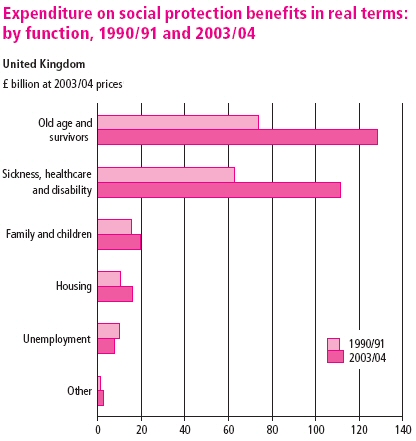
Social protection describes the help given to people who are in need or are at risk of hardship through, for example, illness, low income, family circumstances or age. Central government, local authorities and private bodies (such as voluntary organisations) can provide help and support. The type of help can be direct cash payments such as social security benefits or pensions; payments in kind such as free prescriptions or bus passes; or the provision of services, for example through the National Health Service (NHS). Unpaid care, such as that provided by informal carers, also plays a part in helping people in need. Charities are also a source of social protection assistance in the United Kingdom; the top 500 fundraising charities spent over £2.8 billion in this area in 2003/04!
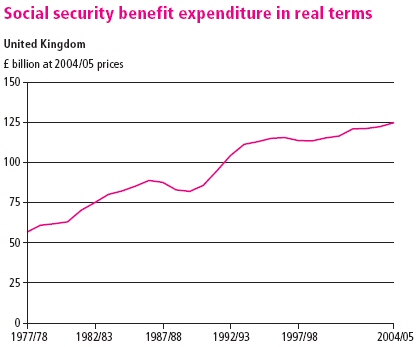
In the United Kingdom, the Department for Work and Pensions (DWP) in Great Britain and the Department for Social Development in Northern Ireland are responsible for managing social security benefits, which include the state retirement pension, disability allowance, income support and pension credit. In real terms, social security benefit expenditure in the United Kingdom has risen from £57 billion in 1977/78 to £125 billion in 2004/05.
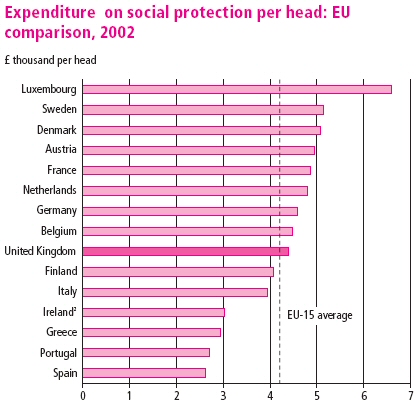
In 2002 UK spending on social protection was £4,400 per person, slightly above the EU-15 average of £4,240 per person.
|
obese |
elhízott |
|
general practitioner |
háziorvos |
learn more:
sources:
National Statistics, UK 2002, The Official Yearbook of Great Britain and Northern Ireland
National Statistics, UK 2005 - Social Trends
Wikipedia, National Health Service
Eyewitness - Travel Guides, Geart Britain, Dorling Kindersley